Dr. Kavya Chandrashekar
Disclaimer : This article contains health related information written by a professional pediatrician, however it is meant for informational purposes only and should not be used as a substitute to individual medical advice.
Table of Contents
Given the speculations that children might be the most vulnerable group during the third wave of COVID-19, as parents and caregivers for children it is natural to go into a panic mode. The best way to face an emergency situation is to be prepared for it.
As part of the preparation for COVID-19 especially in children, I have put together an emergency medical kit that can come in handy especially if your child were to ever suffer from this infection. Do keep in mind that this kit is especially assembled for COVID-19 infection.
1. ORS
Dehydration is the important initial factor that can determine the outcome of any illness. Dehydration means loss of body water along with electrolytes like sodium, potassium, chloride. Lack of body water disrupts the metabolic processes in the body, which in turn produces fatigue.
Younger children are especially at risk because of higher body water content compared to adults, which means with symptoms like vomiting or diarrhea, there is a much larger loss of fluids in comparison to adults. Children also have a higher metabolic rate which means they need higher water content for normal functioning.
Covid-19 in children can present as vomiting and diarrhea with or without fever. Some children can also complain of abdominal pain. It is often mistaken for Food poisoning, also known as Infective gastroenteritis.
The most important component of a COVID-19 emergency health kit is Oral Rehydration Solution (ORS).
ORS is as effective as Intravenous fluids in correcting dehydration and is preferred.
The most common mistake parents make is to use powdered glucose to hydrate their children. Parents need to understand that glucose in powder form provides a rapid source of glucose. It does not correct dehydration nor does it provide electrolytes.
Use either WHO-approved ORS salts or Premixed solutions to correct dehydration. Salts are preferred as they can be used to prepare a larger quantity like 1 liter, as compared to pre-mixed solutions which usually come in a 200ml tetra pack.
Just remember :
- Use boiled and cooled water to prepare Oral Rehydration Solution.
- Once prepared use it within 24 hours, discard any unused solution beyond this period, because of the risk of bacterial contamination.
- Do not store an opened packet of ORS salt for later use. Once open, empty and use the entire content to prepare the solution.
To decide how much total fluids are required by your child use the following calculator below. Remember this is the total fluid requirement of a normal child in a day, which is inclusive of milk or other fluids.
If your child is vomiting or is having loose stools add an additional 100ml as a replacement for every episode of vomiting or diarrhea.
As the formula varies with the weight of the child, use the appropriate calculator.
How much fluids does your child need in a day?
3. Cold and Cough medications
Cold and cough is a sign of respiratory infection. A runny nose and mild or occasional cough can be treated at home successfully with over-the-counter medications.
When it comes to coughing a number of factors decide the need for treatment with appropriate drugs. This might also be a symptom that should prompt you to seek medical advice.
4. Saline nasal drops
Nasal congestion is a very discomforting symptom, especially in younger children. A blocked nose can cause crying, fussiness to feed, inability to sleep.
Saline nasal drops contain saline fluid that helps clear the airway. They are very safe as they don’t have any medications in them. This is often handy in a child with a congested nose.
5. Antiemetics (anti-vomiting medications)
as discussed above COVID-19 can present as a food-related infection commonly termed “food poisoning”, with vomiting and loose stools. As these symptoms can result in rapid dehydration they should be promptly treated at the earliest. Along with Oral rehyration solutions, anti-emetics can help control vomiting.
Often the paradox is that many children find it difficult to keep the medications and fluids down and vomit these as well. In such a case intravenous medications and fluids will be required which may necessitate hospitalization.
Persistent vomiting should be assessed and treated accordingly by a pediatrician without delay.
6. Antidiarrheal medications
Covid-19 can present as isolated diarrhoeal stools with or without abdominal pain.
Probiotics are used for diarrhea and it is extremely important that you avoid medications that are anti-motility like loperamide. Naturally occurring probiotics are present in fermented food items like curd, cheese, fermented soya, etc. Curd or yogurt can be used to supplement with probiotics.
Remember
- Talk to your healthcare professional like your pediatrician regarding dosages for the above medications.
- Label the bottle with Child’s name, dosage, frequency, Expiry date.
Make sure you prepare a separate kit for each child as the dosage of medications can be different for each child.
7. Multivitamins
8. Thermometer
Proper monitoring of a child suffering from COVID-19 infection can be very valuable information that will help your doctor make appropriate decisions.
Pattern and degree of fever can often help doctors determine the type and severity of infection. Low-grade fevers in an active child, who is taking food and fluids adequately can be easily managed at home.
Use the printable chart provided below for easy monitoring.
9. Medical grade mask in the appropriate size
Children infected with COVID-19 can act as a source of infection to close family members. Once your child tests positive it is vital to use a mask to help prevent the spread of infection.
Masks are however not to be used in children less than 2 years because of the risk of choking. Children between 2 and 5 years should be constantly supervised while wearing a mask to prevent any choking-related health hazard.
10. Medicine dispensers like droppers, measuring cups.
Small things like medicine dispensers or measuring cups that are sterilized and ready to use should be kept handy. Important tasks like feeding medicine to a sick child become easier when you have the right device to do it.
11. Pediatric pulse oximeter
Although this is optional equipment, if you can afford one it can be a valuable monitoring device. Most pulse oximeters can tell you heart rate and blood oxygen saturation. If you are treating a child at home a pulse oximeter can be used to determine the need for emergency hospitalization.
Spo2 level of more than 94% is considered normal. Any readings equal to or less than 94% should promptly seek medical attention.
12. Clean cotton towels
These can be used for various purposes like tepid sponging in high-grade fevers to cleaning.
13. Monitoring chart
At-home treatment of children can seem intimidating and challenging. But remember COVID is a viral illness and requires the same care and attention that any other illness needs.
Many a time parents fail to recall accurate milestones in history, like onset and severity of symptoms, which can pose a challenge to doctors in terms of making the right clinical decision. Having a well-maintained monitoring chart can provide doctors valuable information.
This chart is free to download and use.
Free download: Monitoring Chart for At-Home Covid patients
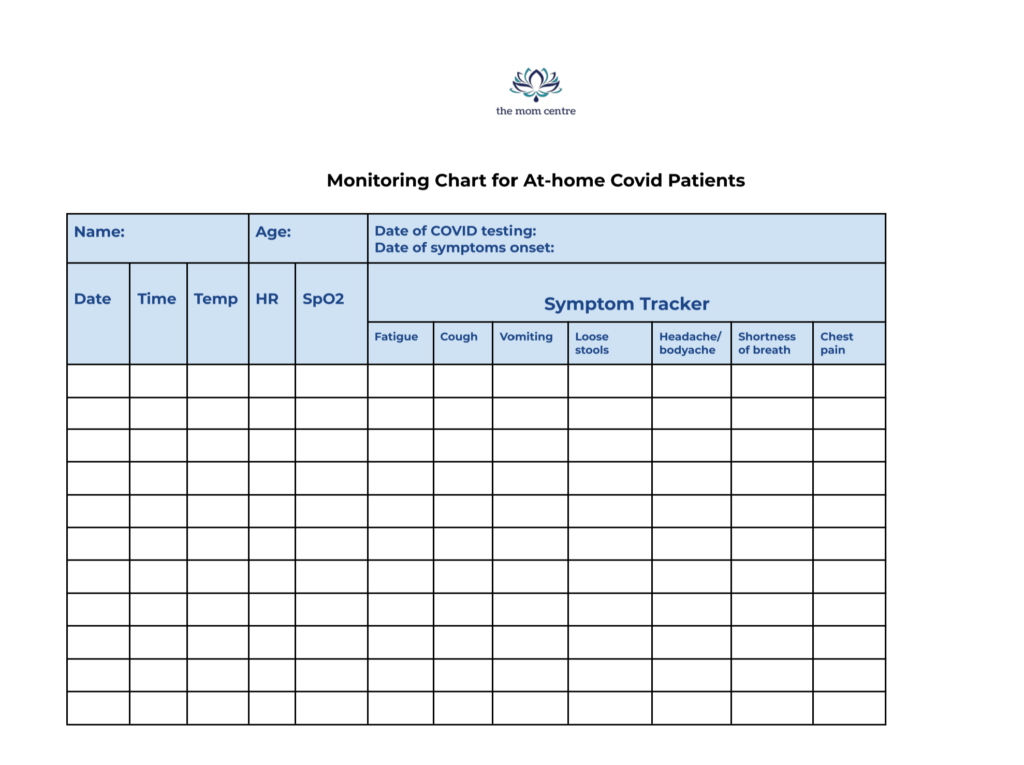
Free Printable monitoring chart for Covid-19 patients for effective monitoring at home
14. Emergency contact information
This should include
- Your child’s health insurance information, preferably a copy of the official insurance card
- List of 5 nearest hospitals covered by your insurance provider*.
- Your pediatrician’s contact number.
* It is always best to make a list of 5 well-researched hospitals that are within 5 kilometers radius, covered by your insurance provider, preferably recommended by your pediatrician. This prevents any avoidable delay in seeking treatment. Always call ahead, explain the condition of the child and your arrival at the hospital. This gives the hospital time to make any necessary arrangements if need be.
15. Important health information related to each child
Many parents often panic when faced with a health-related emergency. In the ensuing anxiety and panic, they often omit vital information like allergies especially the history of previous medication-related allergy and history of long-term medications.
You are likely to forget the names of drugs as well in sheer panic. Preparing a small note with any vital health-related history including any long-term medications that the child is on can immensely help healthcare professionals avoid unnecessary events.
Lastly, remember that “information is power”.
Preparation often gives us the courage to face any emergency.


