COVID-19 symptoms in children: Everything you need to know

COVID-19 continues to spread in our community. However, in comparison to the first wave during which children were least affected, the second wave seems to be affecting children more.
Children are more likely to contract COVID-19 as they play outside with other children who might be carriers without any symptoms, and it might also be due to the fact that children are less likely to follow stringent preventive measures like social distancing, wearing a mask, washing their hands, etc, especially while playing outside. This is especially true when not under the supervision of adults.
Recognizing symptoms of COVID-19 early may be your first step to getting your child tested and following a more active management plan.
Understanding Covid symptoms helps you make decisions with regards to seeking help at the earliest, which is why we have put together a comprehensive guide to what to look for COVID-19 in children.
1. No symptoms at all
Nearly 16% – 50% of the children may not show any symptoms at all. If your child has been in contact with someone who tested COVID-19 positive in the last 14 days, it is important you remain vigilant for symptoms, at the same time it is advisable to get your child tested to prevent spreading infection.
Children are known to be ‘asymptomatic carriers’ and are known to spread the infection to more vulnerable members of the family like grandparents or those with co-morbities.
2. Decreased activity (fatigue) / Decreased appetite level (anorexia)
Even before displaying symptoms like fever or cough, children most likely start showing symptoms like decreased activity and disinterest in regular playtime activities. Parents, especially mothers are really good at picking up subtle changes in behavior in their children.
Younger children may also start refusing feeds and older children may display decreased appetite.
This would be a stage where you have to be extra vigilant, increase fluid intake, provide proper nutrition, and stock up on essential medications.
It is extremely important to prepare a Emergency COVID health kit that might come in handy.
Recent Posts
3. Fever or chills

Fever is a more definitive indicator of any infection in general, Non-Covid as well as COVID. The intensity of fever is not an indication of COVID-19.
Covid is known to produce varying degrees of rising temperature. Some children may have a small rise in temperature while some may have a high-grade fever.
The intensity of fever is not an indication of COVID.
Many children may not manifest fever instead experience chills, especially at the early stages of an infection. Younger children may not be able to vocalize or display these symptoms.
4. Sore throat
Children at different ages manifest this symptom in different ways.
- Older children will be able to tell you a sore throat as pain during swallowing food or while drinking.
- A child over 2.5 to 3 years may be able to vocalise a sore throat as pain pointing towards their neck.
- Younger children who are not able to vocalise may refuse food or become fussy after a few spoons of feed.
4. Nasal congestion or runny nose
Like any other respiratory infection, COVID-19 can present with a runny nose with or without nasal congestion. This in turn can make your child fussy and irritable.
5. Cough: dry or wet
Fever and cough are the most common symptoms of COVID-19. A dry cough is usually indicative of an upper airway infection while a wet cough is indicative of a lower airway or lung infection.
Either way when there is a cough that is persistent it requires a clinical assessment and therefore a consultation with a pediatrician.
Fever and cough are the most common symptoms of COVID-19.
6. Headache or Muscle or body aches
Persistent headache and body ache is more common in older children. This can persist for 10-14 days following COVID infection as well. Younger children may have symptoms like excessive and persistent crying episodes as they cannot vocalize these symptoms.
If your child complains of headaches make sure to ask if they are having neck pain. Neck pain is a red flag symptom and should be assessed by a pediatrician.
7. Loss of taste or smell
Younger children may not be able to appreciate the loss of taste or smell. As these functions help us appreciate food and also stimulate hunger, many children may display decreased appetite.
Older children may be able to vocalize these symptoms. This is an early symptom and many a times the only symptom present.
8. Abdominal pain or Nausea or vomiting or Diarrhea
COVID can present similar to an episode of ‘food poisoning’ with Nausea, Vomiting, or Loose stools. Usually, there is a brief period of Fever or ‘Feeling sick’ period that occurs before the vomiting or loose stools set in, but not always.
If you are unsure of your child’s symptoms, you can check them in Centre for Disease Control’s symptom checker to help you decide whether to seek medical advice.
When should you consult a doctor in person (Red flag signs)
We have seen that COVID-19 can present with a spectrum of symptoms, which are non-specific making it difficult to decide if your child needs further testing or hospitalisation.
However, there are certain symptoms that should prompt you to take your child to a pediatrician on an emergency basis. These are what are termed red flag signs.
Fever persisting beyond 48 hours
Any fever that persists for more than 48 hours should be assessed by a doctor despite giving paracetamol.
Breathing rapidly or Trouble breathing
This is an important and potentially life threatening symptom if not treated properly at the earliest. When there is any pathology that is compromising our lung tissue the body has to increase the number of times we breathe in order to compensate for the compromised lung.
Any child with fever will also breathe faster than usual during the fever episode and breathe normally when fever subsides. But a child who continues to breathe faster even when fever subsides might have compromised lung tissue and will require assessment from a healthcare professional on an emergency basis.
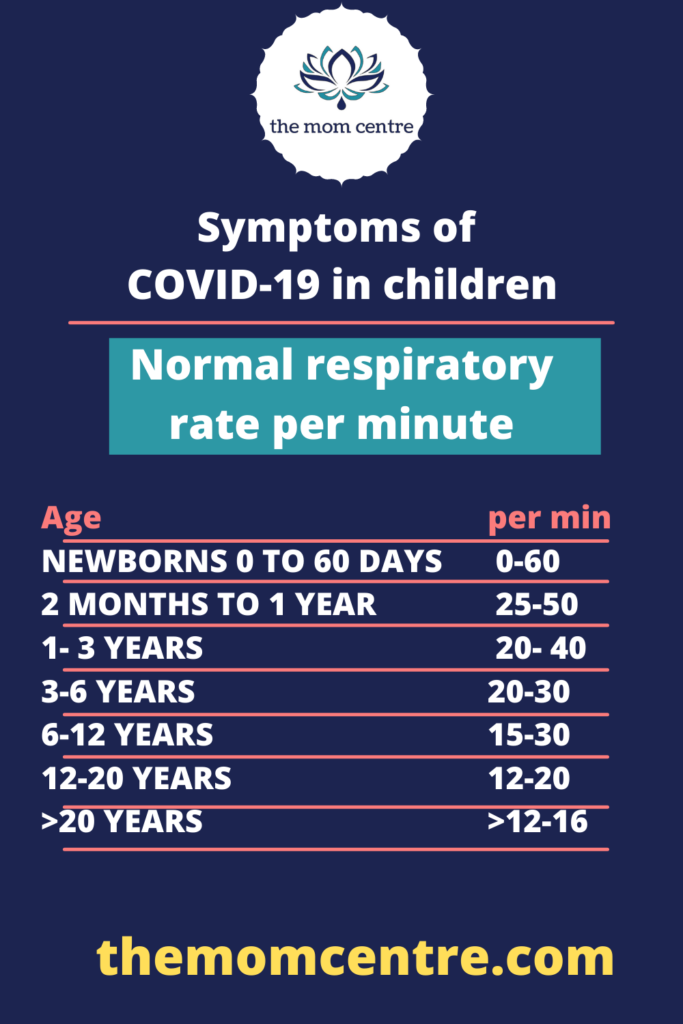
How do I know if my child is breathing faster than normal?
To know if your child is breathing faster, count the number of times your child’s chest moves in and out in a minute. Younger the age the more number of times children breathe. Seek medical help if your child is breathing more than the upper limit or is visibly distressed while breathing.
Persistent pain or pressure in the chest
This must be differentiated from pain while coughing. It is normal to have mild chest pain when you cough especially in the centre of the chest.
But pain, when you take deep breaths towards the sides of the chest may suggest compromised lung tissue. This will usually be accompanied by rapid breathing as detailed above. Any chest pain should prompt you to seek medical advice promptly.
Confusion
A child who seems disoriented or confused is a medical emergency. This should prompt you to seek medical advice in person on emergency basis.
Inability to wake or stay awake
If you find that you find it difficult to wake your child up, your child is drowsy but can be awakened, it might be suitable to seek medical help on an urgent basis.
Pale, gray, or blue-colored skin, lips, or nail beds
Whenever there is any compromise in blood flow or the pressure at which the blood flows, our body compensates by shunting this blood to more important organs like the heart, brain, kidneys, away from the skin which is considered a non-vital organ.
A change in skin color may be a worrisome sign to both parents and doctors. Try warming your child if the room temperature is too cold while you make arrangements to reach the emergency room.
When can you consult a doctor on phone?
Teleconsultation used to be something that many doctors frowned upon, as it doesn’t give us a chance to look and examine the child. Therefore doesn’t give us the confidence to reassure parents about the severity or the diagnosis.
However, with time teleconsultation has proven to be a great triage tool. In a pandemic where lockdowns and restricted travels have become the norm it gives parents an opportunity to talk to a doctor within the safe confines of the house. Based on the initial consultation both the doctor and the parents can make a decision whether to see the child in person or can be managed without having to bring the child to the hospital.
However be warned that it is still an incomplete form of consultation as the doctor is unable to see or examine the child and relies heavily on parent’s ability to give accurate information and conduct self-assessments. This form of consultation needs to be used with caution especially in younger children who cannot speak for themselves.
Here is a list of circumstances when you can use teleconsultation:
- Initial stages of an illness, usually at the onset of fever or any isolated mild symptom.
- A child who is taking at least 70-80% of their regular fluids and food and is generally doing well.
- Symptoms that are getting better
- When you live far away from a hospital and this is your only means of getting health advice
It is also important to know when NOT to use Teleconsultation and see ha healthcare professional in person in a hospital.
Do not use teleconsultation :
- When there are Red flag signs.
- When the diagnosis is unsure.
- For long-term symptoms.
- If you are unsure of providing regular re-assessments and revise decisions
- if you are unsure of providing the necessary care.
What is Multi-system Inflammatory Syndrome in Children (MISC)?
MIS-C is known to be occurring more in children with COVID or those who have been exposed to COVID. It is a disorder that causes inflammation in various organ systems in the body like kidney, heart, lungs, eyes, brain, liver etc.
It can present with symptoms of COVID which progress rather rapidly.
Therefore, the child can develop following symptoms:
- Fever
- Cough/cold
- Vomiting
- Diarrhea
- Severe abdominal pain
- Neck pain
- Conjunctivitis (red, bloodshot eyes)
- Generalised Rashes
MIS-C is still being studied and understood. It is still unclear which group of children are at risk of MIS-C and how it occurs.
If you are in doubt, you can check your symptoms in the CDC symptom checker
Recent Posts